March 14, 2016
Research raises questions on the cause of Alzheimer’s disease
Current thinking on treatment strategies for Alzheimer’s may be called into question following new finding.
Conventional wisdom on the cause of Alzheimer’s disease (AD), and current thinking on treatment strategies, may be called into question by the publication of a scientific paper suggesting that the real culprit may be slow changes to plaque in the brain that simply happen with time.
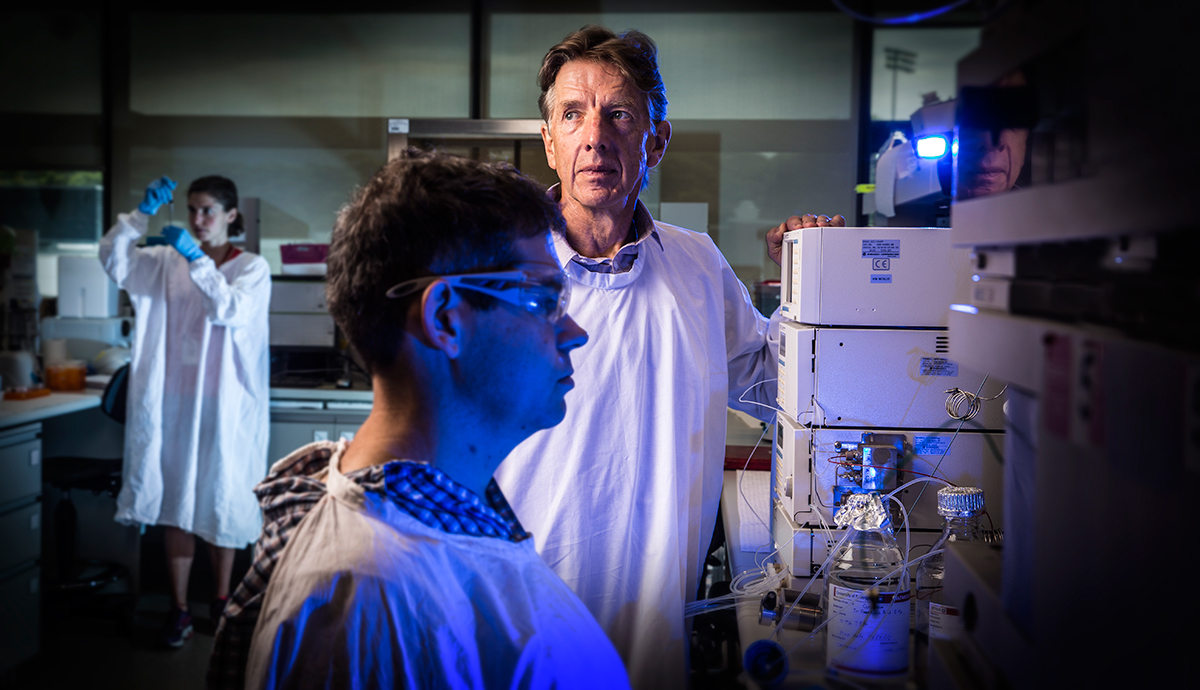
As reported to the journal Analytical Chemistry, researchers from the Illawarra Health and Medical Research Institute, based on the University of Wollongong campus, and the Save Sight Institute at the Sydney Eye Hospital, applied their knowledge and expertise of other diseases of ageing, such as cataract, to examine changes to the composition of proteins in the human brain.
The link between eye health and AD relates to the fact that the human lens contains the highest concentration of proteins of any tissue in the body and altered proteins are associated with a range of age-related pathologies including cataract and AD.
According to the paper’s lead author, Professor Roger Truscott, plaque, which is the key diagnostic feature of AD, forms when the amyloid precursor protein (APP) is cut by enzymes to create smaller fragments called Amyloid beta (Aβ) peptides which are sticky and form clumps that are toxic to brain cells.
To date, researchers and drug companies have focused most of their efforts on clearing two toxic variants - Aβ 1-40 and Aβ 1-42 - but Professor Truscott says that the vast majority of plaque in the human brain is not Aβ 1-40 or Aβ 1-42 per se, but highly degraded or modified versions of these peptides, meaning that current strategies which seek to clear them from the brain may be ineffective.
“These peptides may have been deposited initially, but almost all of them have undergone a large number of changes which make it very difficult for the normal enzymes in the body to break down and dispose of modified Aβ 1-40 or Aβ 1-42,” he said.
“In this paper we show that all of these modifications to Aβ are due to spontaneous processes; i.e. no enzymes are required. These are simply slow chemical reactions that just depend on time and they can all be reproduced in the test tube.”
One conclusion that can be drawn from this study is that the vast majority of peptides within plaque are long-lived; a discovery which could help to explain why many people past middle age have plaque in the brain but seem to suffer no cognitive ill effects.
“It is possible that plaque needs time to become toxic,” said Professor Truscott.
With this knowledge, he suggests that researchers should now investigate the composition of plaque as a function of age in normal human donors as well as in AD patients.
“The majority of AD studies underway are animal studies. What we really need to do is look at how the peptides that make up plaque alter with age and ask if they are different in normal elderly people compared to AD patients and also if they are different in different regions of the brain.
“The next stage of the AD work is to perform these investigations together with research on the toxicity of the various highly modified forms of Aβ 1-40 or Aβ 1-42.”
The research also has significant implications for the development of therapeutics to treat AD, as current strategies focus on the use of monoclonal antibodies to clear plaque from the brain, concluded Professor Truscott.
“Monoclonal antibodies are very specific tools that target certain sites on Aβ. They may not work as well on target proteins that have been highly modified.”