January 27, 2016
Physics research and innovation a lifeline for cancer patients
More than 150 leading Australian and global experts in cancer radiotherapy will converge on Hobart this week at a UOW-led conference to discuss the latest advances in improving cancer treatment.
A major focus for the event is the emerging new technologies and techniques that increase treatment effectiveness while reducing the harmful side-effects, leading to improved patient health and wellbeing.
The two-part conference will start on 26 January with the three-day Mini-Micro- and Nano-Dosimetry (MMND) international workshop, which will focus on aspects of radiation therapy, including the current status of research on new radiation detector technologies for quality assurance in cancer therapy.
It will be followed with the two-day Innovative Technologies in Radiation Oncology (ITRO) workshop on 30 and 31 January. This workshop will present state-of-the-art radiation treatment methods, particularly for cancer of the lung, liver, brain, spine and prostate.
The international event is led by the University of Wollongong’s (UOW) Centre for Medical Radiation Physics (CMRP), a research group that is a world leader in the development of quality assurance radiation devices instrumentation and methods that ensure patients receive the correct dosage
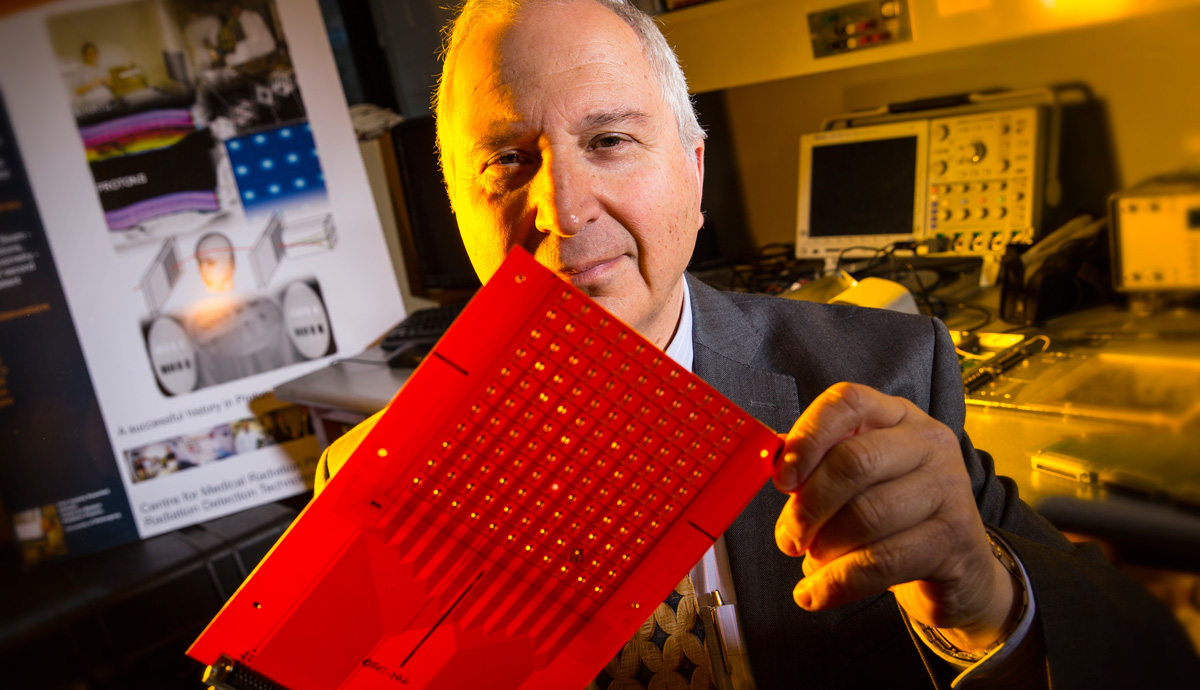
Distinguished Professor Anatoly Rozenfeld who is a founder and Director of CMRP has led the development at CMRP of several radiation detection systems that are currently in use in clinical practice.
Among the innovations to be presented is a new type of radiation skin-dose detector being developed by Dr Marco Petasecca from CMRP.
The tiny device comprises a wafer-thin, square-shaped material about the size of a thumbnail that contains silicon diodes. These diodes react to the radiation and send measurements to the clinicians in real-time.
Several detectors could be placed on the patient’s body to create a ‘map’ of the radiation dosage.
“The skin is thinner than a piece of paper - too much radiation and the patient will suffer irritation, much like a harsh sunburn, and discomfort following treatment,” Dr Petasecca explained. “If the dose is reduced there is the risk the malignant cells will not be completely destroyed.
“When doctors treat breast or prostate cancer, the curvature of the body complicates their calculations of the dosage required and how much radiation is hitting the skin.”
Prototype detectors that are cheap to make, re-usable and work with standard hospital equipment, have been successfully trialled in the lab and will soon move to pre-clinical trials in a hospital environment.
“At the moment, doctors use a film to detect radiation, but this is double the thickness of the human skin, leading to inaccurate results. It also takes 48 hours after treatment to show results. Our detector works in real-time and treatment could be stopped if the dosage is too high.”
Professor Rozenfeld said the biennial event was an important biannual forum that brought together world leaders in cancer treatment.
“Events such as this are how we get to the next step in improving cancer treatment with radiation,” he said. “Despite the advances of the past decade, there is still a great deal of uncertainty in treatment planning and quality assurance.
“Special attention will given to new radiation oncology modalities including proton and heavy ion therapy, which are emerging technologies and not yet implemented in Australia.”
“We are constantly working on ways to precisely calculate the dosage amount, develop detectors to ensure we are hitting the target with precision and not harming the patient, as well as building our understanding of the fundamentals of how radiation affects human cells.”