April 29, 2020
Australians wary of using Big Data analytics to track infectious disease
Study shows community wants transparency, data security and public oversight of disease surveillance systems
As Australians debate the pros and cons of downloading the Federal Government’s COVID-19 tracking app, new research has found that while people were marginally in favour of using Big Data analytics to detect and control infectious disease outbreaks, they did hold serious reservations.
Many participants in the study were concerned about the loss of privacy involved – especially if the technology involved analysis of mobile phone GPS tracking data or social media use to monitor peoples movements and social interactions (neither of these characteristics that are features of the COVIDSafe app).
More broadly, participants did not trust governments to run secure and effective technological systems, and were even more suspicious of private sector access to disease surveillance data.
The study, led by researchers from the University of Wollongong (UOW) and published this week in BMC Medical Ethics, looked at community views on the benefits and risks of technologically enhanced communicable disease surveillance systems. It was conducted prior to the coronavirus outbreak.
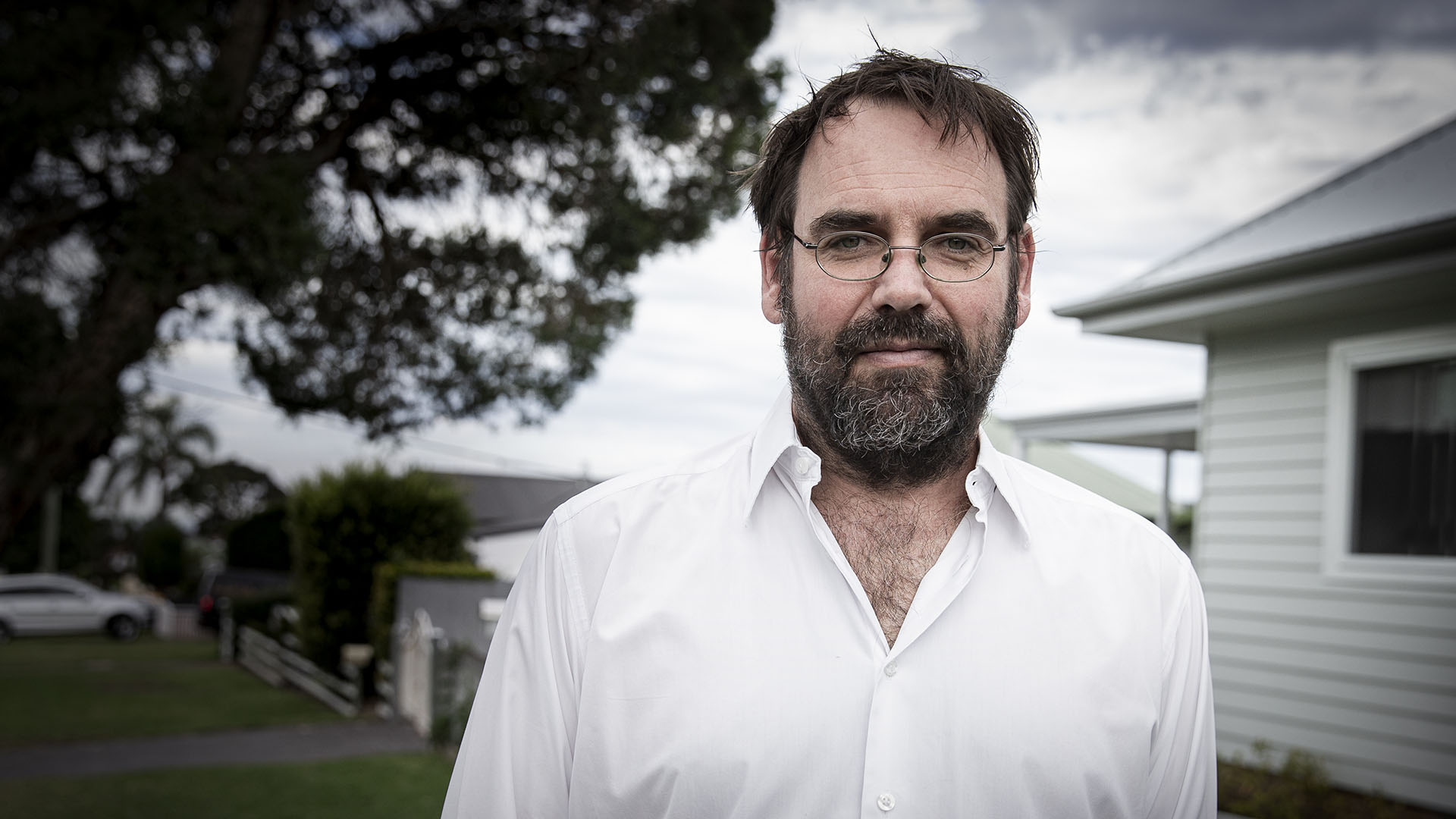
Lead author Dr Chris Degeling, from UOW’s Australian Centre for Health Engagement, Evidence and Values (ACHEEV), said two new technologies – pathogen whole genome sequencing (WGS) and Big Data analytics – had potential to improve our capacity to detect and control outbreaks earlier, saving lives and resources.
“Depending on the accuracy and comprehensiveness of the data collected, the potential benefits of enhancing surveillance systems with both of these technologies include more rapid detection and response to infectious disease outbreaks,” Dr Degeling said.
“With pathogen WGS especially, health authorities can more easily identify disease clusters, identify transmission direction, and link otherwise unrelated cases.”
However, using these technologies to capture more detailed and specific personal information could be seen as intrusive and a threat to privacy.
To understand community attitudes, researchers from UOW and the NHMRC Centre for Research Excellence in Emerging Infectious Disease (CREID) convened four community juries that were demographically diverse and in different regions of NSW.
Experts with different perspectives on the potential benefits and costs of technologically enhanced public health research and communicable disease surveillance presented the juries with balanced factual evidence. Jurors were also able to questions the experts.
Most jurors supported the introduction of data linkage and WGS for public health research, provided standard practices were applied to prevent individuals from being identified. However, allowing this information to be operationalised as a surveillance system was highly contentious. Three juries voted in favour and one against, all by narrow margins.
For those in favour, support depended on conditions related to system oversight and security being met. These included voluntary participation, public oversight, data security, and penalties for non-compliance or misuse.
Those against were concerned about loss of privacy and did not trust Australian governments to run secure and effective systems. Any suggestion of private sector involvement or commercialisation of WGS or surveillance data was unanimously rejected.
“Most jurors were not concerned about governments accessing personal data for controlling and preventing infectious disease outbreaks,” Dr Degeling said. “The main reservation were about maintaining security of the data, keeping it in Australia and ensuring that it would not be used to generate wealth for private interests.”
The uptake and acceptance of Bluetooth-based contact tracing apps on mobile phones has been promoted as a component of an effective and proportionate response to the COVID-19 pandemic. This study shows that introducing new surveillance systems can be controversial because of a lack of public trust, even when the potential public health benefits are clear.
“I am not surprised about the current debate as the COVIDSafe app has been released without much public consultation,” Dr Degeling said.
“Trust is hard to gain and easy to lose. Without clear mechanisms for the public to oversee and establish the trustworthiness of the underpinning systems, the COVIDSafe app may be a bridge too far for a significant proportion of the Australian public.
“However, given the current circumstances, I suspect many jurors would be in support of using the app as almost all of them found the potential for technologies to enhance outbreak responses to be very compelling, but were reluctant for these types of systems to operate in the background when the threat was low.”
The study also suggests conditions that may increase public willingness to accept such surveillance systems.
“The study highlights how establishing trustworthy systems of governance are essential for the social license of these types of enhancements to communicable disease surveillance practices,” Dr Degeling said.
“Making sure the system is sustainably funded, transparent and accountable, and that it represents and is responsive to broad public interests, are key to the perceived legitimacy of using these technologies when there is not a public health emergency.
“The current circumstances highlight the importance of introducing formal systems for public oversight of new surveillance technologies such that the practices and data uses entailed are transparent and acceptable to the public.”
ABOUT THE RESEARCH
‘Community perspectives on the benefits and risks of technologically enhanced communicable disease surveillance systems: A report on four community juries’ by C Degeling, SM Carter, AM van Oijen, J McAnulty, V Sintchenko, A Braunack-Mayer, T Yarwood, J Johnson, and GL Gilbert is published in BMC Medical Ethics.
The research was funded by the National Health & Medical Research Council of Australia.