September 22, 2015
Crunching the numbers for better cancer care
Study shows best locations for radiotherapy treatment centres to deal with growing need for cancer care.
Tyranny of distance leads to close to one in six cancer patients in New South Wales not receiving vital radiotherapy treatment, data modelling by researchers at the University of Wollongong SMART Infrastructure Facility has revealed.
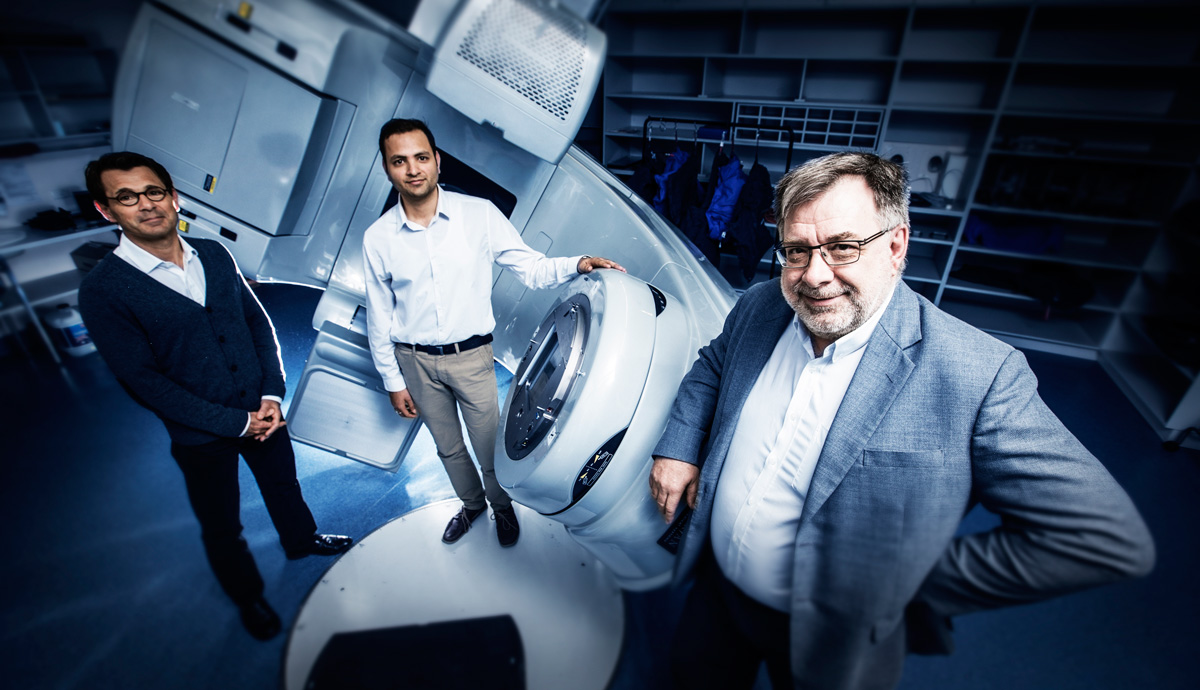
This finding led researchers, in collaboration with Professor Andrew Miller from the Illawarra Cancer Care Centre, to develop a predictive software tool that will help health planners decide the best locations to build future radiotherapy treatment units to more effectively deal with current and growing need for cancer care.
Rather than focus on raw population numbers and historic cancer rates, the data-modelling project used three criteria to aid general efficiency, service availability and equality.
Efficiency requires a base population of about 250,000 people to justify spending on a radiotherapy unit; availability is the number of people living within 50 kilometres or less from an existing treatment centre; and equity/equality ensures people with fewer financial resources still get treatment.
Professor Miller said health policy decisions should be informed by data as opposed to “expert opinion” that often overlooked equity in favour of maximising population coverage.
“The data arbiters cannot just be about financial and operational efficiency if the distance issues are to be overcome. Placing a linear accelerator in a more remote area will lead to reduced efficiency. It is the inevitable price of access.
“Obviously if you refuse to build anything but a fully utilised department, availability will suffer because those without access will remain without access.”
To address the complex and interconnected problem, Dr Nagesh Shukla said the planning of efficient and accessible cancer radiotherapy services at a regional level required the use of population predictions, cancer rates, and mapping tools to estimate the number of patients living within different travel distance bands from radiotherapy centres.
“Our research showed that supply of radiotherapy services significantly lags behind what we calculated to be optimal demand. This trend is only going to continue into the future if new centres are not appropriately established,” he said.
“The key question then becomes where is the best place to locate new services, particularly given the costs involved and when there are multiple locations that want better health care. To answer that question it’s important to look at the profile of the communities.
“For example, the proportion of elderly people will steadily increase over the next decades due to increased life expectancy and the population of ‘baby boomers’ who are entering the high cancer incidence period. This will increase the number of cancer cases.”
Australian Institute of Health and Welfare (AIHW) cancer data indicate the average cancer rate at local government area level was 612 per 100,000 people in 2011, which is predicted to increase by approximately 30 per cent to 805 cases per 100,000 people in the next decade.
The most recent additions to cancer treatment in the region have been new linear accelerators at the Shoalhaven Hospital in Nowra in November 2014, followed by an additional unit at Wollongong Hospital in December 2014 as part of a multi-million dollar expansion to the Illawarra Cancer Care Centre.
The SMART modelling suggested that prior to the new linear accelerator, close to 400 people living within 50 kilometres of Nowra town centre required treatment in Wollongong. Anecdotal evidence suggests that the Nowra centre is likely already catering for this amount of patients, indicating the underlying and potentially underestimated demand for health services.
The team credited the collaborative approach that draws on knowledge and methods from disciplines outside medicine - such as analytical methods for production systems and industrial engineering - to help address public health issues.
“Each specialist brings to the table unique characteristics of creativity and ingenuity derived from life, study and experience,” Professor Miller said. “For this reason, collaboration is the only answer to solve problems.”
The research was recently published in the journal Computer Methods and Programs in Biomedicine.