[Professor Gordon Wallace]: The AIC Centre of Excellence for Electromaterials Science and ANFF Materials Node have forged the partnership that enables fundamental discoveries to be translated into practical devices in the shortest time possible. When scientists, engineers and clinicians are empowered to create structures containing multiple materials using simple fabrication tools, extraordinary things can happen and they are happening right now.
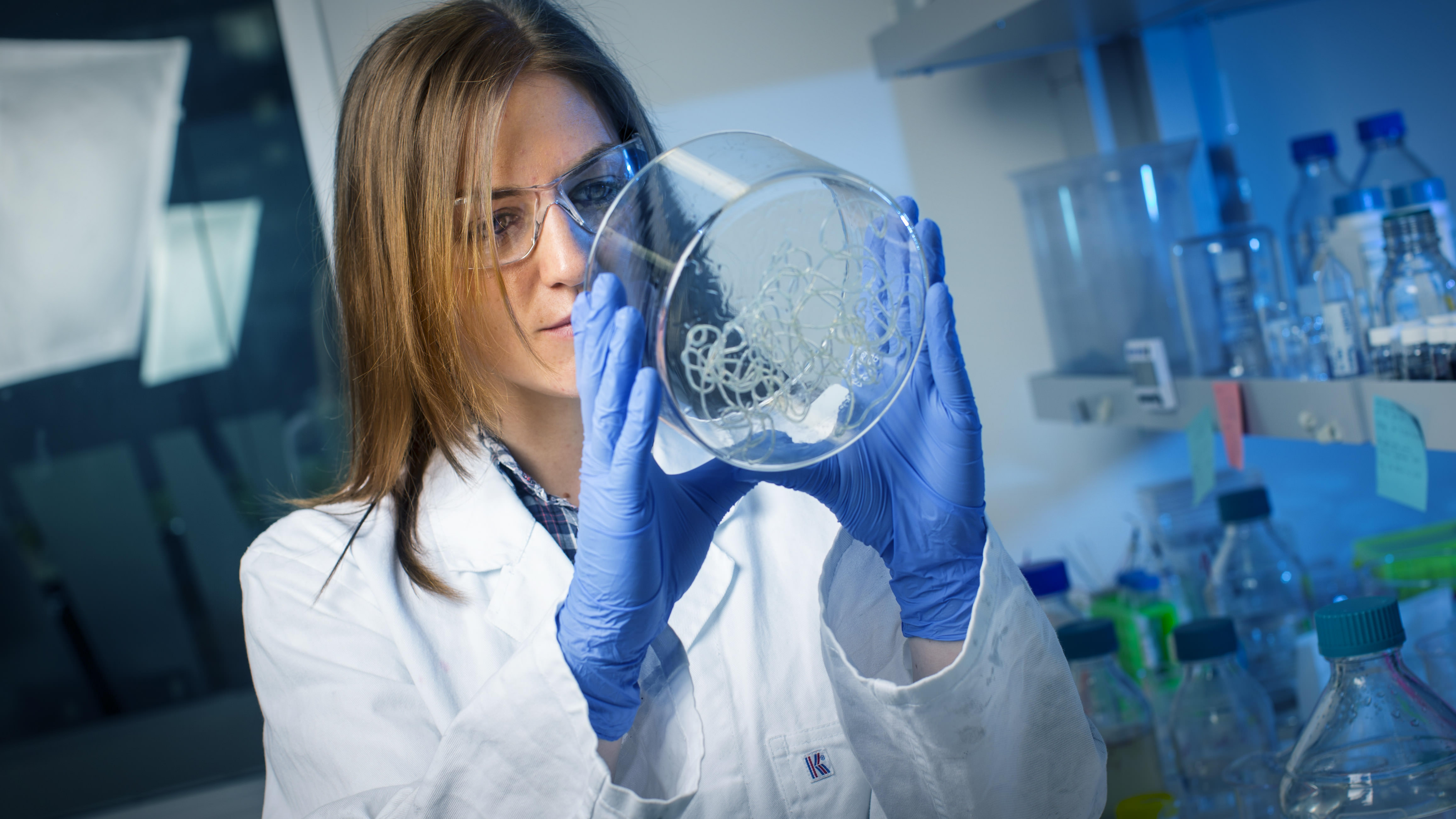
[Professor Peter Choong]: What we're trying to do and what we've actually succeeded in in our laboratories is isolating certain cells from the patient and helping these cells move down the pathway to developing the patient's own garbage. So structures that you can 3D print that we then populate with the patient's own stem cells become the types of structures that we can implant into these defects of cartilage. Arthritis which affects about half of patients or people over the age of 65 may have as its origin an injury in the distant past. These injuries can leave defects that lead to the development of Arthritis. This type of project that we're doing looks at repairing those defects by scaffolds and stem cells in the hope of recreating exactly the sort of cartilage that is now missing. And if we can do that recreating a smooth surface for the joint that matches perfectly with the other side of the joint, we have a fighting chance of firm helping slow down the progress of Arthritis.
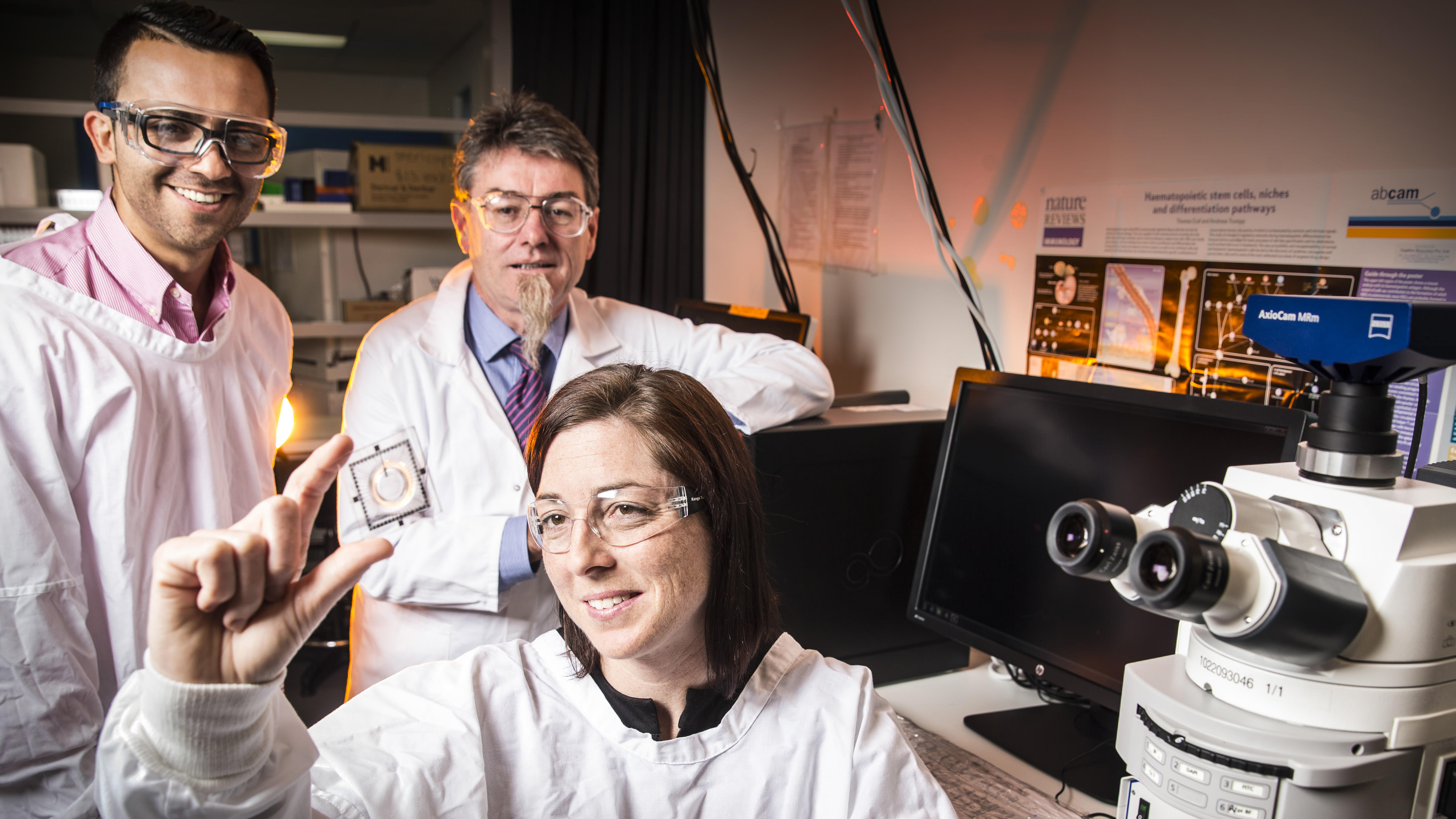
[Professor Gordon Wallace]: Using the combined skills of ACES and ANFF Materials Node we have now developed Novel ink formulations consisting of biomaterials. These enable 3D printing of Adipose stem cells with a high survival rate and also facility at their development into functional cartridge. Effective delivery of the stem cells that the biomaterial required the development of a coaxial printhead to provide further protection to the cells during the printing process. A handheld version of this, the Biopen was developed for surgery.
[Professor Peter Choong]: As a surgeon, we are in surgery with the patient's part open to us. And what we would like to do is actually sculpt out an area to fill the defect in the carnage for example. The Biopen is such a perfect instrument for this because held in the surgeons own hand is a device that not only delivers the ink that fills the defect, it has another tube running right next to it that also delivers the cell. Being able to use this real-time means we can be as patient specific as we can in order to repair the defect in the college.
[Professor Gordon Wallace]: This holistic approach to the challenge at hand required the skills of scientists, engineers and clinicians with access to world-class facilities. The ANFF/ACES partnership provides all of this. If your business needs access to these skills and facilities or as interested in developing new technologies through partnerships, contact us. If you are interested in being trained in a highly multidisciplinary environment and acquiring the skills to take fundamental advances into practical structures and devices, contact us. The ACES / ANFF partnership is helping existing industry explore new opportunities and creating new manufacturing industries. It is providing personnel with the skills to facilitate these.
[Music]