Cancer. It’s a word we all fear. But with today’s medical advances, come cancers are significantly easier to treat or even curable. However, one of the most complex kinds that we still struggle to treat is brain cancer.
Our brains are our most sensitive organ encased in a protective shell. Surgery to remove a tumour there can sometime be all but impossible and the protective blood brain barrier makes use of chemotherapy exceptionally difficult.
Our only viable option, then, is external beam radiation therapy but even that has shortcomings. To properly treat brain cancer, we are inflicting significant damage to some very sensitive tissues that surrounds the tumour. And we know that this, particularly in children can lead to hormonal, growth and cognitive issues. And even still, the five-year survival rate for brain cancer has not changed in 30 years.
So how can we treat such a difficult disease? My solution is the use of an alternative radiation source. A synchrotron. A synchrotron produces light radiation that is exceptionally powerful and very fast. To put this into perspective, the radiation dose delivered at a synchrotron is over 5000 times faster than what we can deliver in a hospital.
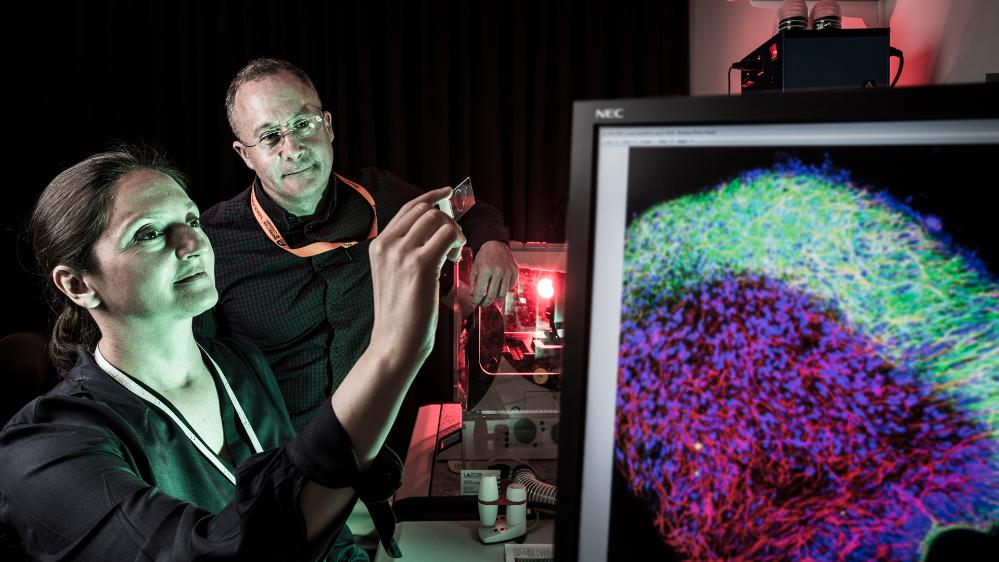
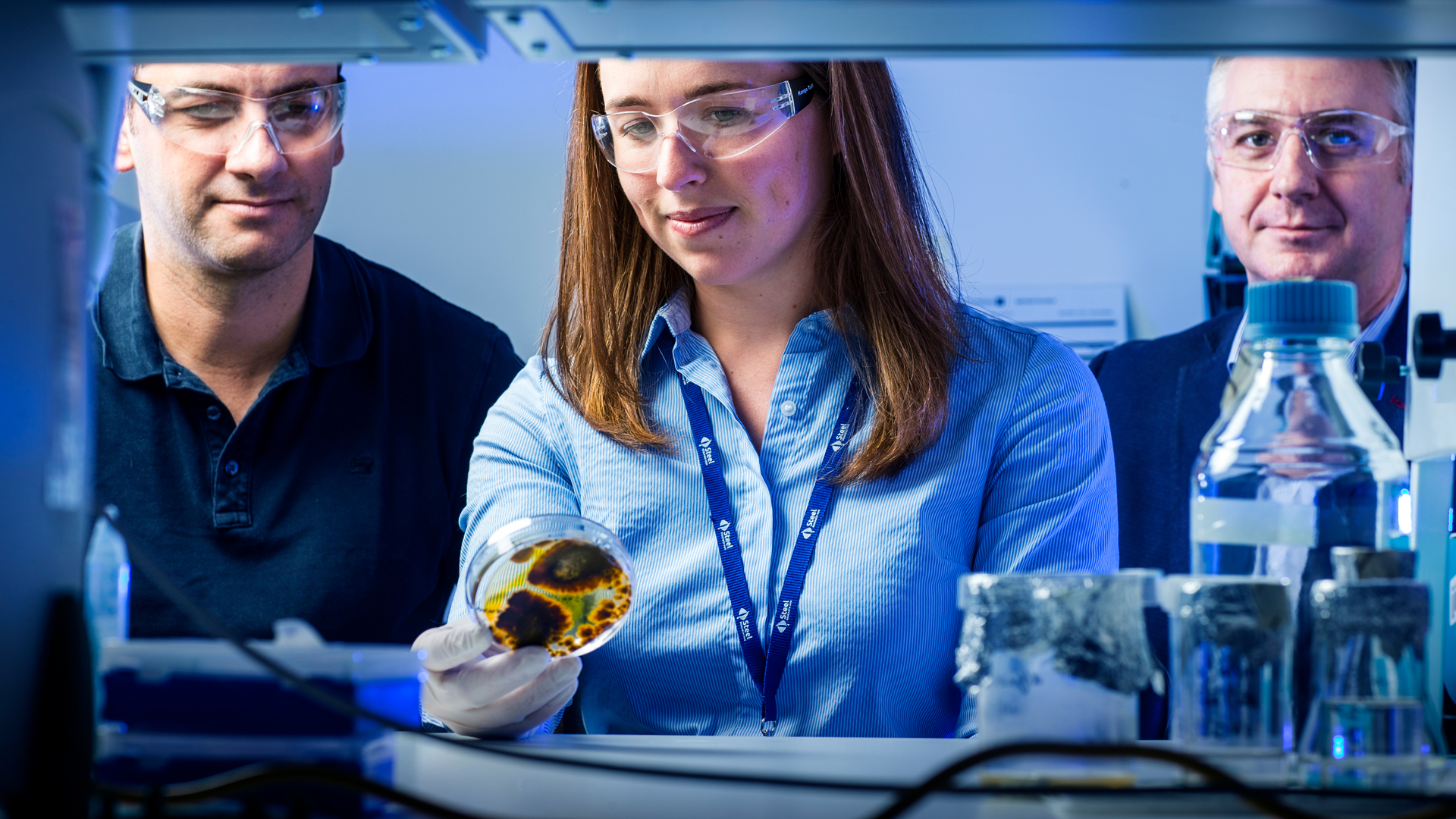
This fast radiation is critical to treating difficult cancers. But we can do even better than this. We can insert a collimeter, which is essentially a cone. This form sour beams into peaks of exceptionally high dose and valleys of significantly lower dose. This is microbeam radiation therapy, or MRT. MRT is powerful – the peaks of the beams sever the tumour like a knife, while the healthy tissue is essentially unaffected. But we can improve this even further. We can add nanoparticles directly to the tumour. Nanoparticles which are tiny specs of metal interact with the MRT to produce extra radiation that is specifically localised to the tumour. This means we can selectively increase the damage delivered to the tumour and further decrease the dose delivered to the surrounding healthy tissue.
Nanoparticles, combined with our knife-like beam, and the speed we can deliver the radiation, means we can treat the tumour with just one shot. This is exceptional, compared to current hospital treatments which require daily radiation for many weeks.
This April, we treated rats with brain cancer with this exact method. Without treatment, the cancer causes death within 20 days. With our one shot treatment, we have a quarter of our cohort remaining at 100 days and counting. This is proof that we are laying the foundations to finally curing brain cancer.